In a fully globalised and digitised world, people are facing an ever-increasing onslaught of complex information. The human mind is not prepared for the exponential growth of technological change. So with mental health disorders already on the rise, staying sane – i.e. maintaining and restoring our mental health – will become one of humanity’s primary challenges. So, how does the mental health landscape look like? Over 10% of the global population live with a mental health disorder. Even pre-COVID, studies and reports have already pointed out that mental healthcare systems are struggling to adequately address people’s needs.
What we are seeing is only the tip of the iceberg

In the best healthcare systems…
- 10% of people receive care from a psychotherapist or psychiatrist
- 30% of people diagnosed with a mental health disorder only receive care from a GP
- 60% of people with a mental health disorder remain undiagnosed and uncared for
For example, the following data points illustrate the mental health landscape in Germany:
- High prevalence: A fourth (27,8%) of the population in Germany suffers from a mental disorder in a given year.
- Shortage of psychotherapists: Even though the number of psychotherapists increased by 44% between 2009 and 2018, this rise is not enough to keep up with the rapidly growing demand for psychotherapeutic treatment, which exceeds existing capacities. In 2009 only 2.76% of the German population had contact with a psychotherapist. In 2018 that number had already jumped to 3.89% (a total of 3.221 million people). Adjusted for demographic effects, this corresponds to an increase of 41%.
- Long waiting times: Due to the shortage of psychotherapists and the rising demand, the average waiting time to start treatment is 5 months (19,9 weeks).
- Costs: The annual direct health economic costs due to mental illness in Germany amount to 44,4 billion €.
- COVID-burden: A recent survey conducted by the German Psychotherapists Association showed that patient inquiries in practices increased by an average of 40% compared to the same period in 2020.
Mental health landscape in the United States
Germany is not the only country in the world that is facing these challenges. According to a 2017 report from the Kaiser Family Foundation, published in the Journal of the American Medical Association, one in five US adults and kids have a mental health or substance abuse issue.
It’s a bigger disease burden in the United States than cancer or heart disease, but just 40% of adults and 50% of kids get help. The reasons for this are manifold. Some people are too embarrassed or afraid to reach out. But other common reasons found by the Kaiser Family Foundation line up with the significant psychiatrist gap—people who couldn’t get help didn’t know where to turn, they couldn’t afford care or their insurance didn’t cover it.
Implications of the pandemic for the mental health landscape
The status quo and the associated insights illustrate the massive challenges we already have in mental healthcare.
However, the COVID-19 pandemic has had an unprecedented impact on humanity and the mental health landscape. Firstly, the COVID-19 crisis made it much more difficult or even impossible for people to meet their therapists and counsellors in person. Consequently, many of those already in treatment were unable to receive the support they needed. Secondly, people seeking help, found it much more difficult to enter the care system as many institutions continue to operate with limited capacity. Moreover, early warning signs of a Mental Health Tsunami are being reported.
The long-term impact on mental health is still not fully foreseeable but the demand for psychological support is rising by the day because of fear and anxiety about COVID-19, emotional distress resulting from illness, bereavement, unemployment, income loss, and loneliness due to social isolation. These determinants are all interacting, and generating or intensifying mental health problems at a global scale.
A Kaiser Family Foundation Health Tracking Poll from July 2020 found that many US adults are experiencing specific negative impacts on their mental health and well-being, such as difficulty sleeping (36%) or eating (32%), increases in alcohol consumption or substance use (12%), and worsening chronic conditions (12%), due to worry and stress over the coronavirus.
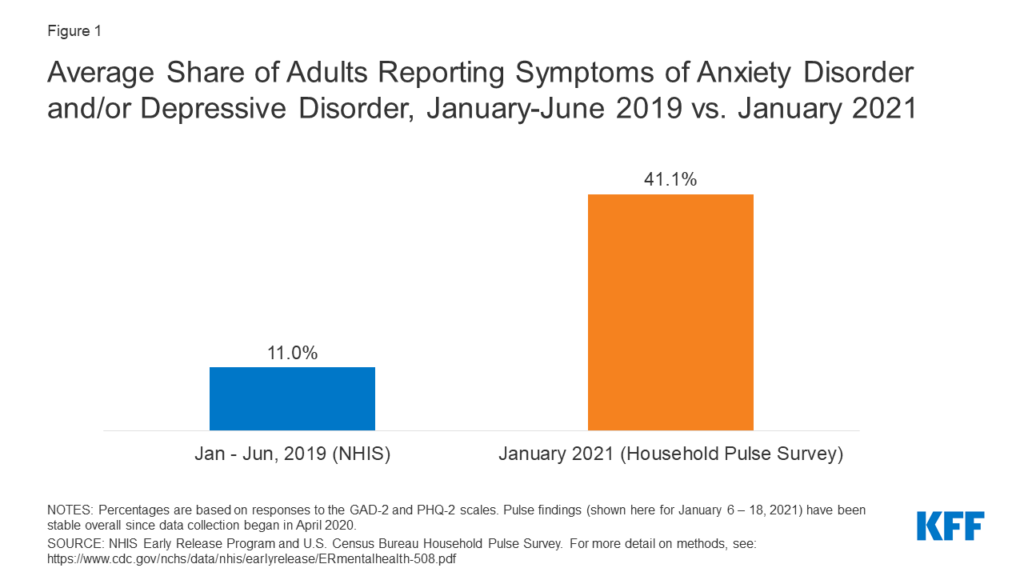
In January 2021, 41% of US adults reported symptoms of anxiety and/or depressive disorder, up from one in ten adults between January to June 2019 (Figure 1). Among adults reporting symptoms of anxiety and/or depressive disorder, more than 20% report needing but not receiving counseling or therapy in the past month during the pandemic.
Given the pandemic’s implications for both people with pre-pandemic or new mental health conditions, the crisis highlights the barriers to accessing mental health and substance use disorder services.
In addition, a recent study analysed the neurological and psychiatric outcomes of COVID-19 survivors. The largest study to date, which was published in ‘The Lancet Psychiatry’, analysed electronic health records of 236,379 COVID-19 patients mostly from the United States to adequately assess the effects of COVID-19 on brain health. The results indicate that one in three COVID-19 survivors (34%) were diagnosed with a neurological or psychiatric condition within six months of infection.
The most common diagnoses after COVID-19 were anxiety disorders (occurring in 17% of patients), mood disorders (14%), substance use disorders (7%), and insomnia (5%).
The researchers outline that these diagnoses were more common in COVID-19 patients than in flu or respiratory tract infection patients over the same time period, suggesting a specific impact of COVID-19.
Five ways to reinvent mental health care
What needs to be done to provide sufficient mental health support? So far, accessing mental health care is often associated with different challenges for patients, such as long travel and waiting times, associated costs, and limited mobility due to physical impairment or old age.
Hence, five aspects are vital to improve the landscape of mental health and create sustainable and patient-centered support.
1Low barrier access
Research shows that time spent seeking healthcare represents a burden to already vulnerable patients, and results in lost productivity to employers and society, and a potential inefficiency within healthcare systems. As a result, providers need to offer patient-centered and easy access to their mental health services, covering the full patient journey.
2Speed initial treatment contact
The vast majority of people with lifetime disorders eventually make treatment contact, but it often comes with a delay of several years as shown in studies in the United States, Netherlands, Argentina and by the World Health Organization. As interventions to speed initial treatment contact are likely to reduce the burdens and hazards of an untreated mental disorder (typically described as “chronification”), healthcare systems and providers should focus on respective measures and services.
3Prevention is crucial
In Germany, some of the patients who come to see psychotherapists suffer from typical symptoms, but are not showing a severe mental health condition or illness yet. Consequently, most of these people remain untreated. What they would need, though, are prevention programmes and support so as to prevent them from actually becoming mentally ill and needing treatment.
4Empowerment first
People with mental health problems would like to deal with their mental stress and symptoms on their own first before reaching out to a professional for help, research found. Hence, patients need to be empowered and supported with the appropriate resources and services during that stage.
5Technology-based support of employee mental health
The Third Annual Workforce Attitudes Toward Mental Health Report, compiled data from 1,229 US full-time workers and over 150 CEOs to understand the views and behaviors toward mental health of employees and their most senior leaders, one year through the pandemic. 96% of CEOs believe they are doing enough for employee mental health, but only 69% of employees feel the same.
48% of US employees report experiencing high to extreme stress over the past year – a 7% increase over the last two years. Yet, the number of employees who have used technology-based mental health support has increased significantly by 66% over the same time period. More than three-quarters of employees who worked with a mental health professional did so virtually in the past year.
However, the increased focus on mental health will not be sustainable if the existing mental health solutions are not accessible. Digital mental healthcare is able to provide this continuous access and support employee mental health.
Digital mental health: the new normal
The status quo and the pandemic’s implications point out challenging times for the whole mental health landscape.
Digitisation offers the opportunity to address the highlighted five aspects with new pathways and tools to reinvent and improve the existing mental health landscape. The COVID-19 pandemic has led to unprecedented use of technology in mental healthcare, such as telehealth, digital therapy programs or apps for behavior change. According to research, millions of people unable to access traditional services have sought help from digital mental health providers.
US-based Ginger, which offers text-based mental health coaching, teletherapy and psychiatry, reported that usage increased 159%, and virtual therapy and psychiatry was up 302% in September 2020 compared to pre-COVID-19 averages. Ginger’s psychiatrists have written 163% more prescriptions for psychotropic drugs, primarily for antidepressants, as compared to pre-COVID-19 averages.
UK’s Kooth plc service, which runs virtual mental health services on behalf of the National Health Service (NHS), has seen an increase of 34% in young people and 53% in adults seeking support digitally.
HelloBetter offers ten scientifically validated psychological online courses for prevention and treatment (digital therapeutics). In 2020 alone, the client growth increased by 320%.
These examples illustrate promising new approaches to providing more patient-centered support, and complements existing structures in the mental health landscape. It is unlikely that we will see a full return to traditional in-person mental health service models. The ability to provide more flexibility to a traditional system and the potential for more cost-efficient, scalable and even effective delivery of support, underlines the potential of digital mental health.
We hope that this article was insightful for you! We will be sharing each of our articles on our LinkedIn page to further engage with the HelloBetter community. Hence, we invite you to share your perspective on this topic and post your experiences in the LinkedIn comments.
Click here for the related LinkedIn post!
We are looking forward to exploring with all of you how digital mental health solutions will redefine the future of care.
About HelloBetter
HelloBetter is a global pioneer in the field of digital mental health. No other provider worldwide has conducted as many clinical studies on the effectiveness of its online mental health courses. With our unrivalled scientific expertise (30+ RCTs) and passion for supporting people with mental health problems, we have already helped tens of thousands of patients to lead better lives. Find out more about HelloBetter on our Company page.
With HelloBetter Insights we want to share our learnings and analysis with the broader mental healthcare community. Every week, we will survey the ecosystem, report on promising developments, but also highlight the tough challenges that the industry is facing.
