Digital mental health programmes are an effective instrument to address mental health disorders such as depression. Currently, however, most formats still follow a “one-size-fits-all” approach: options to react dynamically to the unique needs and development of each individual are limited. In our large-scale research project “MAIKI”, we used cutting-edge technology to open up the black box of digital depression treatment. The three-year project, conducted in collaboration with renowned digital mental health and AI researchers, was recently completed. Some of our main achievements and findings are presented here.
The “Digital Phenotype”: Toward A Data-Driven Model of Mental Health
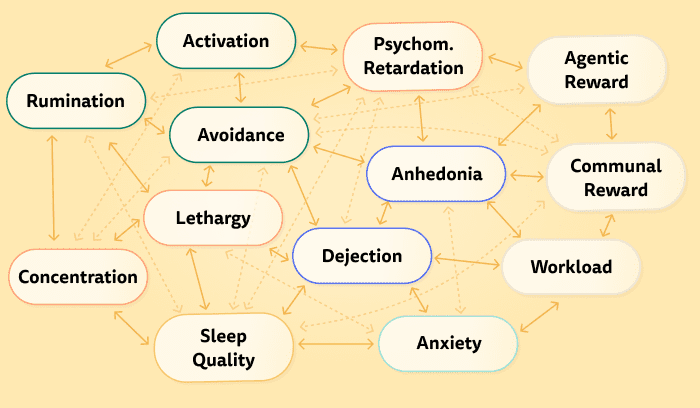
Mental disorders are not unchanging monoliths; they are complex, individual patterns of feelings, thoughts, and behaviors that evolve dynamically over time. In psychological and psychiatric research, it is increasingly recognised that we must focus on individual networks of symptoms and behaviours to understand mental disorders, and to provide better-personalised care (Hofmann & Curtiss, 2018).
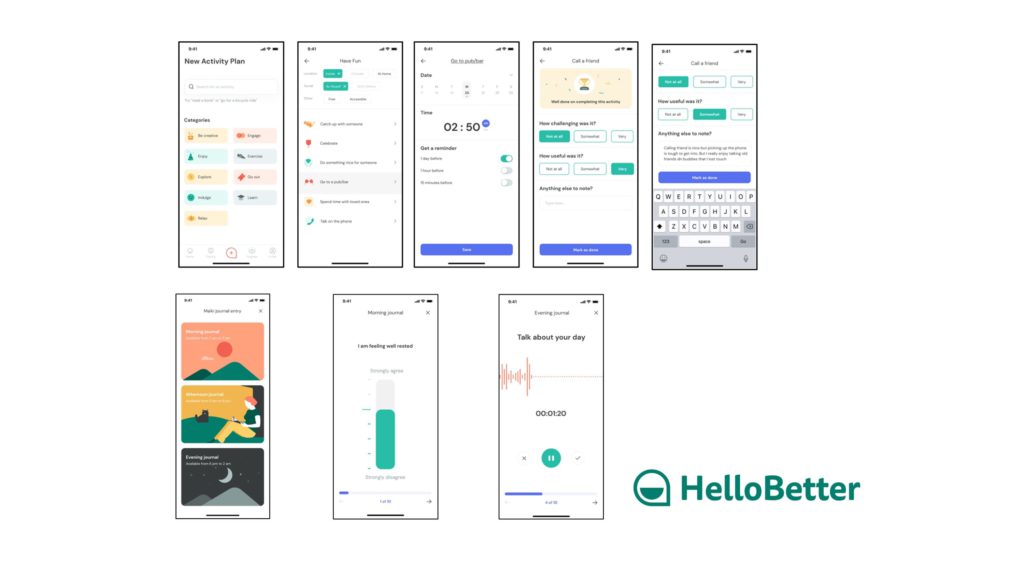
As part of the MAIKI project, we developed a technical infrastructure using novel advances in sensor and affective computing technology to create a personalised, data-driven model of each patient’s mental health. In a real-world study, we combined this infrastructure with HelloBetter’s Depression Prevention course to generate a “digital phenotype” of each patient’s depressive symptoms.
One strength of digital mental health applications is that they allow the collection of an unprecedented amount of fine-grained temporal data. Digital phenotyping is an emerging research field in which this “digital fingerprint” is used to model symptoms and behaviours associated with mental disorders and to predict their development over time (Montag, Sindermann & Baumeister, 2020). In our MAIKI study, the following modalities were used to achieve this goal:
- Mobile sensor data: unobtrusively captured information such as GPS patterns and phone usage are known to predict psychological states and feelings (Rohani et al., 2018). In our infrastructure, this input is used to derive moment-by-moment behavioral patterns associated with depression.
- “Ecological momentary assessment”: structured journaling is a typical part of psychological treatments of depression. Besides the therapeutic rationale, daily self-assessments also allow us to obtain an understanding of the “ups and downs” in patients’ symptoms.
- Voice features: breakthroughs in AI research now make it possible to derive subtle indicators of an individuals’ mood via recordings of their voice (Schuller & Schuller, 2020). As part of the MAIKI study, we also explored how this novel data modality can be used to predict depression.
“Knowing Me, Knowing You”: The Benefits of Personalised Machine Learning
Using these various modalities, a dense time series representative of individuals’ mental health is generated. This allows us to apply state-of-the-art machine learning architectures such as recurrent neural networks (RNNs) with gated recurrent units (GRUs) to predict and forecast symptoms of depression.
A common problem with machine learning approaches in (mental) health care settings is that clinical heterogeneity is not sufficiently considered; both in terms of patients’ individual symptomatology, and how they respond to treatment. Therefore, we employed different personalised machine learning approaches that pay greater respect to the unique, “idiographic” mental health patterns that individuals display over time.
One example of personalised machine learning we applied is transfer learning with shared common layers (e.g. Taylor et al., 2017). In this deep learning architecture, a common backbone neural network is used to capture overall patterns. Then, personalisation layers are added, allowing the model to “attune” itself to the individual. We found that, using this and other personalisation approaches, the predictive performance of a state-of-the-art RNN could be improved by 20%. Forecasts of depressive symptoms in the future were improved by roughly 12%.
This means that, using this personalisation strategy, we can better understand individuals’ current and future symptoms than previous, already very powerful AI architectures were able to do. This allows to provide “precision digital mental care”, meaning the right type of help for the right person, at the right moment.
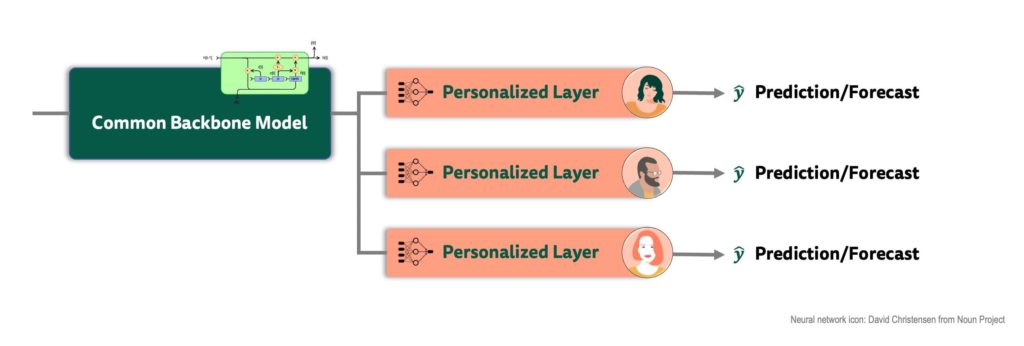
In digital health, fairness is a crucial desideratum. Data-driven technology should not inadvertently introduce bias concerning any protected patient characteristic (e.g. gender, age or ethnicity). Machine learning models often work better in some patient groups than in others which may reinforce existing disparities (Gianfrancesco et al., 2018). Therefore, we also examined the fairness of our models, and how personalisation may help to reduce existing biases. We found that personalisation all but eliminated differential performances, in our case concerning the biological sex.
We also paid attention to personalising course content, for example by developing a recommendation system for positive activities based on calculated recommendation scores.
“The Naked Truth”: Limitations & Ethical Considerations
Our findings underline the potential of digital phenotyping and personalised machine learning in digital mental health care contexts. Nevertheless, limitations and ethical considerations must be considered. The results of the MAIKI study are promising, but more research in clinical populations is needed to examine if our sensing infrastructure can be safely implemented into programmes at scale.
Digital phenotyping involves the collection of highly sensitive personal data. Rigorous data privacy and transparency standards must be maintained in clinical practice to ensure that patients are in control of what they want to share at any treatment stage.
Final Thoughts
For us at HelloBetter, research is a crucial part of our DNA. In the past three years, the MAIKI project allowed our company to go into a deep dive about how we can use technological innovations to create a digital mental health care infrastructure for the future. We are very grateful for the fruitful cooperation with leaders in the field of affective computing and AI in the last years, for example Professor Björn Schuller (University of Augsburg and Imperial College London). For us, the MAIKI project is a big step towards reaching our ultimate goal: creating intelligent, engaging and effective digital therapeutics for individuals suffering from mental health problems such as depression.
Results of the MAIKI project will be published in peer-review journals. This project was funded by the Federal Institute of Education and Research (BMBF, FKZ13GW0254). Preliminary findings based on parts of the project data can be found in a preprint by Kathan et al. (2020).
Literature
Gianfrancesco, M. A., Tamang, S., Yazdany, J., & Schmajuk, G. (2018). Potential biases in machine learning algorithms using electronic health record data. JAMA internal medicine, 178(11), 1544-1547.
Hofmann, S.G. & Curtiss, J. (2018) A complex network approach to clinical science. European Journal of Clinical Investigation, 48:e12986. https://doi.org/10.1111/eci.12986
Montag, C., Sindermann, C., & Baumeister, H. (2020). Digital phenotyping in psychological and medical sciences: A reflection about necessary prerequisites to reduce harm and increase benefits. Current Opinion in Psychology, 36, 19-24.
Rohani, D. A., Faurholt-Jepsen, M., Kessing, L. V., & Bardram, J. E. (2018). Correlations between objective behavioral features collected from mobile and wearable devices and depressive mood symptoms in patients with affective disorders: systematic review. JMIR mHealth and uHealth, 6(8), e9691.
